News Category: Oral Polio Vaccine (OPV)

The environment
Dar es Salam refugee camp, in Bagassola district, Chad, is home to thousands of refugees. 95% of the population is Nigerian, displaced by years of violent insurgency, drought and insecurity in the Lake Chad basin. Some have lived in the camp since 2014.
Here, temperatures soar to 45 degree Celsius nearly every day. Dust is inescapable, colouring everything a shade of yellow. Houses are constructed from tents, tarpaulins and reeds, pitched onto sand. There is no employment, few shops, and no green areas.

Kilometers from the lake, residents have no access to the water around which their livelihoods revolved, as fishing people, as traders at the markets located around the island network, or as cattle farmers. This renders them almost entirely reliant on aid. The edge of the camp is an enormous parking lot, filled with trucks loaded with donations. Signs interrupt the landscape, attributing the camp’s schools, football pitches, and water stations to different funding sources.
Polio immunization is a core health intervention offered by the health centre here, with monthly house to house vaccination protecting every child from the virus.
“We vaccinate to keep them healthy”
In return for their work, vaccinators receive a small payment, one of the few ways of earning money in the camp. In Dar es Salam, there are thirty positions, currently filled by 24 men and six women, and applications are very competitive. Those chosen for the role are talented vaccinators, who really know their community.

Laurence speaks multiple languages, adeptly communicating with virtually everyone in the camp. He is a fatherly figure, engaging parents in conversations about the importance of vaccination whilst his colleague gives vaccine drops to siblings. Their mother is a seamstress, constructing garments on a table under one of the few leafy trees. Laurence engages her in conversation, explaining why the polio vaccine is so important.
Describing his work, he says, “I tell parents that the vaccine protects children from disease, especially in this sun, and that we vaccinate every month to keep them healthy.”
A precious document in a plastic bag
Chadian nationals living in nearby internally displaced persons camps don’t have the same entitlements as international refugees. Several hours’ drive from Dar es Salam, children lack access to even a basic health centre.

At a camp in Mélea, vaccinators perform routine immunization against measles and other diseases under a shelter made from branches. Cross-legged on the ground, they fill in paperwork, carefully administer injections, sooth babies, and dispose safely of needles. Other vaccinators give the oral polio vaccine to every child under the age of ten. These children are mostly from the islands, displaced by insurgency. Their vaccination history is patchy at best, and it is critical that they are protected.
One father arrives accompanied by his small, bouncy son. As the baby looks curiously at the scene in front of him, his dad draws out a tied plastic bag. Within is his son’s vaccination card, carefully protected from the temperatures and difficult physical environment of the camp.
A UNICEF health worker reads it, and realizes that the child is due another dose of polio vaccine. Squealing with confusion, the baby is laid back in his sibling’s arms, and two drops administered. The shock over, he is quickly back to smiling, rocked up and down as his dad folds up the card, and ties it up in the bag once more.

“Our biggest challenge”
Back in Dar es Salam, DJórané Celestin, the responsible officer for the health centre explains the wider challenges of vaccination in this environment.
“We don’t just vaccinate within Dar es Salam in our campaigns. We are also responsible for 27 villages in the nearby surroundings. Reaching these places proves our biggest challenge.”
Away from the main route to Dar es Salam, there are no roads or signs, and many tracks are unpassable. To reach the 539 children known to live in the villages, vaccinators walk, or rent motorbikes, travelling for many hours.
This month, another round of vaccination in the Lake Chad island region concluded. Hundreds more refugee and internally displaced children are protected, in some of the most challenging and under-resourced places to grow up.


Three-year-old Ibrahim wouldn’t stop crying. Suffering from ringworm, a fungal infection, his leg had become badly infected. Left untreated, he risked developing fever and scarring wounds.
For Ali Musa, his father, it was hard to know where to turn for help. Where he lives, in the nomadic community of Daurawa Shazagi in the Nigerian state of Jigawa, there is little access to professional medical treatment.
From his home, it would take Ali a full day to trek to the nearest primary health centre. He does not recall the last time anyone in his community made this “practically unthinkable” journey.
Reaching all children with vaccines
“But when I heard in the market that a medical team was coming to us to treat sick people, especially women and children, I went with the hope to at least get him some relief from the pain,” Ali recalls.
There, Ali met members of the mobile health teams supported by the UNICEF Hard-to-Reach (HTR) project – funded by the Government of Canada’s Department of Foreign Affairs, Trade and Development. These teams are helping to ensure that children receive polio vaccinations, whilst also providing basic health services – including medications to fight infections like ringworm – in hard-to-reach areas of Nigeria.

The teams vaccinate against measles, meningitis and other diseases, and provide vitamin A supplements and deworming tablets for children. They also carry out health promotion activities, teaching communities about important practices such as exclusive breastfeeding. During each clinic, members of the HTR team give two drops of polio vaccine to every child, ensuring that all are protected from the virus.
At the end of their visit, the team pack up the clinic, and travel home, taking hours to cross difficult terrain by foot, boat and motorbike.
2390 children vaccinated
The HTR project aims to reduce the immunity gap among children living in Nigeria. Since 2016, when cases of wild poliovirus last were detected in the country, determination and commitment have helped to strengthen eradication efforts, but many states still face an uphill task to increase historically low routine immunization rates. This is especially the case in rural areas, where there are few services, and communities have to travel far to the nearest health clinic.
So far in 2018, the project has reached thousands of previously unvaccinated children with the life-saving polio vaccine, including 2390 children in Ibrahim’s state, Jigawa.
“Why should I let anything stop me?”
Salamatu Kabir, who leads a HTR team assigned to take immunization and basic health care services across Jigawa, says “I look at it this way. If people from outside can come all the way to bring the hard-to-reach project to my country, why should I let anything stop me from delivering it to my own people who are most in need?”
A retired health worker, she says that she doesn’t think twice about the many hurdles that she will have to overcome to reach children in communities like Ali and Ibrahim’s.
Far more of a concern is planning meals for her four children whilst she is away, and packing all the equipment she will need for the journey. Experience over the years has taught her what items to add to her bag besides vaccines. She always carries an umbrella, an extra pair of clothes, insect repellant and depending on the season, either an additional pair of sandals or, most often, rain boots.
Salamatu asserts that for the team members, “visiting the settlements to administer health care is something we have come to love and look forward to”.
When the team finally does arrive at their destination they are greeted by an expectant community. Salamatu is motivated by the direct impact her work has on the lives of others.
Little Ibrahim is one of those to benefit. After treatment from the team, his condition improved quickly. His father Ali has since become a volunteer for the HTR project, and an avid advocate within his community for medical care.
“I will do my best to ensure every child in my village benefits from the help that is coming from far,” he says.

Following identification last month of an acute flaccid paralysis (AFP) case from which vaccine-derived poliovirus type 1 (VDPV1) had been isolated, genetic sequencing of two VDPV1s from two non-household contacts of the AFP case has now confirmed that VDPV1 is circulating and is being officially classified as a ‘circulating’ VDPV type 1 (cVDPV1).
The National Department of Health (NDOH) of Papua New Guinea is closely working with the GPEI partners in launching a comprehensive response. Some of the immediate steps include conducting large-scale immunization campaigns and strengthening surveillance systems that help detect the virus early. These activities are also being strengthened in neighboring provinces.
The GPEI and its partners are continuing to work with regional and country counterparts and partners in supporting the Government of Papua New Guinea and local public health authorities in conducting a full field investigation, risk assessment and to support the planning, implementation and monitoring of the outbreak response.
For more information:
Contact Oliver Rosenbauer, Communications Officer, Global Polio Eradication Initiative, tel: +41 79 500 6536
Related resources
A 34-month old child had presented with symptoms of acute flaccid paralysis (AFP) on 29 April, from a community with low vaccination coverage in Orinoco delta, Delta Amacuro state.
A Sabin type 3 poliovirus was isolated from stool samples of the child. Isolation of Sabin type 3 poliovirus can be expected in children and communities immunized with bivalent oral polio vaccine, which contains attenuated (weakened) type 1 and type 3 Sabin strains. Final laboratory analysis received today has confirmed that the AFP symptoms are not associated with wild or vaccine-derived poliovirus.
A number of conditions or infections can lead to AFP, poliovirus being just one of them. As part of global polio surveillance efforts, every year more than 100 000 AFP cases are detected and investigated worldwide. Clinical evaluation of the child is underway to determine the cause of the paralysis. The most important point is that the child should be provided with appropriate care and support.
While wild and vaccine-derived polio have both been ruled out as the cause of this child’s symptoms, this area of Venezuela is experiencing vaccination coverage gaps. It is critical that countries maintain high immunity to polio in all communities, and strong disease surveillance, to minimize the risk and consequences of any eventual poliovirus re-introduction or re-emergence.
The partners of the Global Polio Eradication Initiative (GPEI) – WHO, the US Centers for Disease Control and Prevention, Rotary International, UNICEF and the Bill & Melinda Gates Foundation – will continue to support national and local public health authorities in these efforts, together with the Pan American Health Organization, which serves as the Americas Regional Office of WHO.
For more information, please contact:
- Media team
PAHO
Tel: +1 202 974 3440
Email: mediateam[AT]paho[DOT]org
- Oliver Rosenbauer
Communications Officer
Global Polio Eradication Initiative
WHO Geneva
Tel +41 (0)79 500 6536
Email: rosenbauero[AT]who[DOT]int
An acute flaccid paralysis (AFP) case, a symptom which is caused by a number of different diseases (polio being just one of them), is currently being investigated. The child is 34 months old, and had onset of paralysis on 29 April, from an under-immunized community in Orinoco delta, Delta Amacura state.
A Sabin type 3 poliovirus was isolated from stool samples of the AFP case, and is being further analysed, including to determine if the paralysis was caused by the isolated strain. Final laboratory results are expected next week.
Isolation of Sabin 3 poliovirus is not unusual, and can be expected in children and communities immunized with bivalent oral polio vaccine, which contains both attenuated type 1 and type 3 Sabin strains. As part of global polio surveillance efforts, every year more than 100,000 AFP cases are detected and investigated worldwide.
WHO’s Pan American Health Organization (PAHO) and the GPEI continue to support local public health authorities in conducting an epidemiological and field investigation into this event.

Almost everyone in the Killa Saifullah district of Balochistan, Pakistan, knows and respects 35-year-old Taj Muhammad. A dedicated and passionate doctor by profession, Dr Taj spends his days working as a Union Council Medical Officer in his local public health facility, and his evenings running a free medical clinic for local residents.
In his capacity as Medical Officer, he coordinates polio eradication efforts at the Union Council level, which is the smallest administrative unit in Pakistan.
His role includes coordinating microplanning, training frontline health workers, and supervising polio vaccination campaign activities. Since the start of his medical career in 2007, he has supervised more than 100 polio vaccination campaigns.
Dr Taj says he became a doctor to fill the existing health care gap in his area. “During my childhood, my mother was seriously ill and she died because of the absence of medical facilities in our area. She often used to tell me that I must become a doctor to help poor people with their health. She died afterwards but her words are still in my heart,” he explains.
His hometown, Killa Saifullah, is located 135 kilometers away from Balochistan’s provincial capital Quetta. Economic and social deprivation is widespread, and the district lacks basic health facilities, particularly for women and children. “There is only one hospital, serving only 150 people per day in the district, whereas the current population is more than 200,000. In these conditions, working as a medical officer is quite challenging,” Dr Taj says.
His job is tiring, and the demands are huge, but Dr Taj perseveres. As well as supporting polio vaccination activities, and endorsing vaccination, each day he tends to the large crowd of people who gather outside his evening clinic, often desperately needing health care.
His work to serve his community is particularly important because Killa Saifullah lies close to Dukki, where the only case of polio in Pakistan so far in 2018 was reported. Nawabzada Dara Khan, who chairs the Killa Saifullah’s Municipal Committee, notes that the community feels “vulnerable” knowing that the virus is close by.
Since the first polio case of 2018 was detected, polio vaccination campaigns have been conducted in response in all neighboring districts, including Killa Saifullah. But whilst this has increased immunity to the virus, it has also caused vaccine hesitancy amongst some parents, who question the need for multiple vaccination campaigns.
“We are trying hard to vaccinate each and every child; however, repeated campaigns and misconceptions are posing a big challenge for us,” Dara Khan says.
Luckily, the efforts of dedicated doctors like Dr Taj are helping to remove misconceptions and doubt. With the immense trust and respect he enjoys from his community, he has been able to use his free evening clinic as a local platform to advocate for polio eradication and the safety of the vaccine, extending his critical role in the polio programme.
Dara Khan adds, “The contribution of Dr Taj in polio eradication is commendable. His goodwill is playing a very positive role within our community to remove these misconceptions.”
His impact is also wide ranging, reaching multiple different families.
The proof? In April, thanks to the intensive efforts of Dr Taj and others, no parents or caregivers in Killa Saifullah refused vaccination.
That’s 70,690 children who now have lifelong protection from polio.


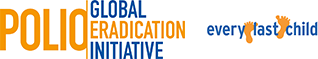
How do vaccinators ensure that every child is reached?
Every child needs to be vaccinated to protect them from poliovirus. To achieve this, detailed plans are prepared for vaccination teams. The aim is to find each child under 5 years of age – in Afghanistan, that’s around 10 million – and to reach them with vaccines.
A heavy steel gate opens on a quiet suburban street in central Herat. The city lies in a fertile river valley in Afghanistan’s west, an area rich with history. Over the centuries, invaders from Genghis Khan’s army to the troops of the Timurid empire, the Mughals and the Safavids have opened the gates to rule the city once known as the Pearl of Khorasan.
Now, a far more peaceful group can be seen walking down the streets of Herat. Equipped with blue vaccine carrier boxes and drops of polio vaccine, the teams knock on one door after another to vaccinate any children they find inside. The aim is to eradicate polio in Afghanistan.
Four-year old girl Fariba peeks from behind the gate and steps out on the street, followed by her father Mashal.
Mashal encourages his daughter to open her mouth to receive two drops of polio vaccine, and a drop of vitamin A. Fariba looks at the vaccinators with suspicion, but follows her father’s guidance.
The vaccinators thank them and continue down the street.
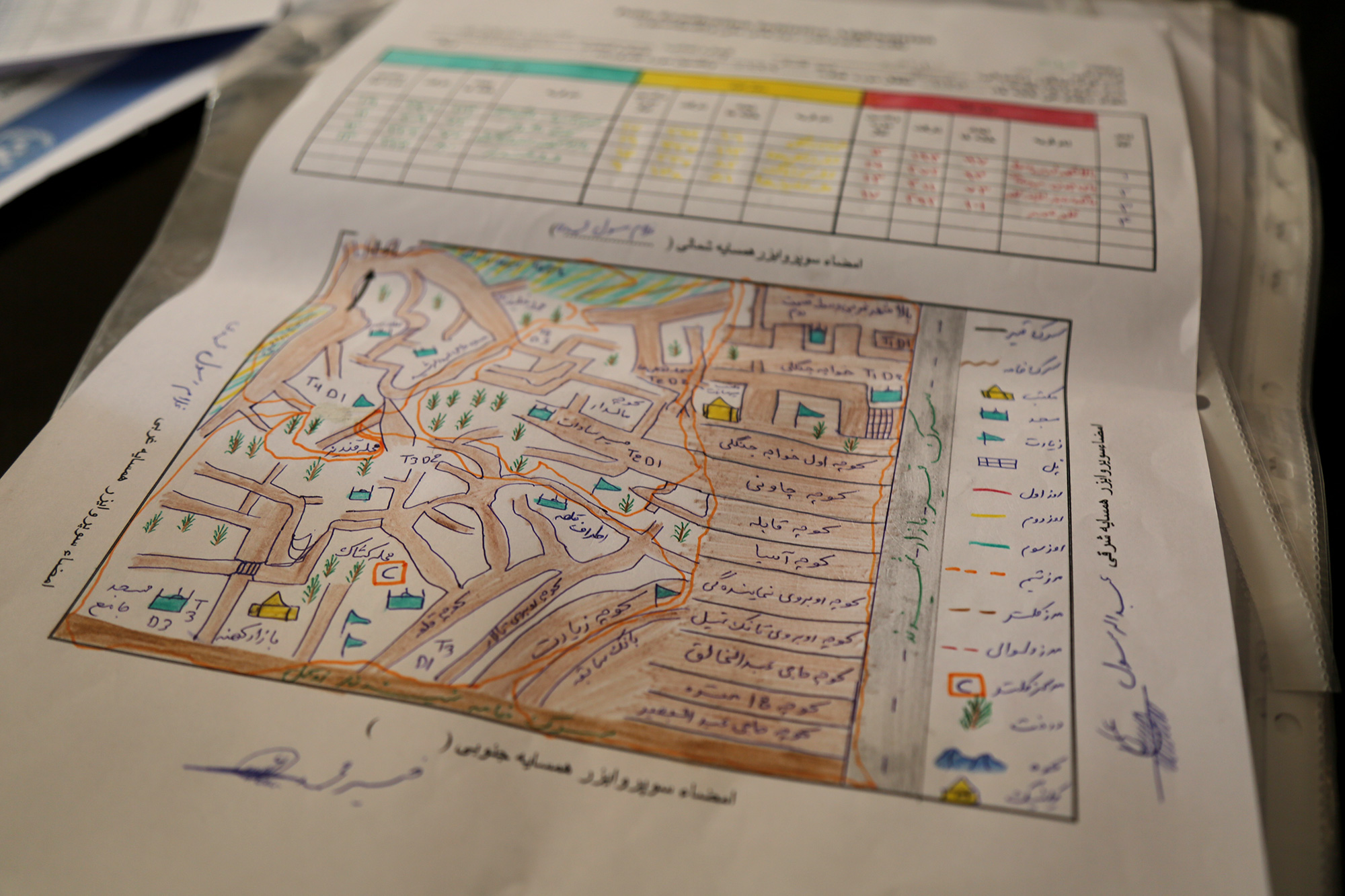
Locating all children
In March, vaccinators in Herat gave oral polio drops to over 150 000 children.
In a country with one of the highest rates of population growth in the world and frequent population movement, it is no easy feat to tell how many children live in each province, district, village, block, house or tent.
How do vaccinators know where the children in each area are located then? Through a simple but elegant guide known as a ‘microplan’. This is what the vaccinator follows: Where to start the day, how many children live on that street, which is the next house to visit?
No coincidence: Who goes where
A few kilometres from Fariba and Malik’s home, Dr Khushal Khan Zaman is sifting through printed plans on his desk at the World Health Organization office.
Dr Khushal explains that once a year, health workers physically count the houses in their area. Then they check that the plans from the previous year still match the numbers.
Campaign supervisors know the approximate number of children in each house from the last campaign. But the data is complemented by their personal knowledge. As locals, they often know of any changes in the composition of their community – where new children have been born, or the location of nomadic groups who have settled in the area.
This helps keep the plans accurate. For instance, if a nomadic group has stayed in an area for a longer time, their tents may be added to the microplans. For shorter stays, a separate checklist is used instead to monitor nomadic population movement. This improves the programme’s ability to trace and reach every child with vaccines, even if they are on the move.
Once the plans have been updated, teams of vaccinators are assigned to visit specific homes on a particular day during the upcoming campaign.
The final plan indicates not only the numbers of houses and children, but also details on how many related items are needed for each team: vaccine vials, vaccine carriers, ice packs (to keep the vaccines at optimum temperature), chalk, tally sheets, pens, leaflets, finger markers, plastic bags and scissors.
This is a contrast to a few years ago, when the plans listed only the name of the area with the estimated number of children to be vaccinated. The newer plans include even the smallest houses, and information on the closest mosque and local elders.
“It needs to be clear to everyone, which team is responsible for which area. We mark where the teams start and which direction they take using arrows,” Dr Khushal explains.
And it is no coincidence who goes where. To ensure that parents allow their children to be vaccinated, vaccinators may be allocated parts of their community that they know well, to increase trust when they deliver the vaccine.
Children like Fariba might not understand yet why the vaccine is important, but their father does. When vaccinators knock, it is not chance that brings them, but care and commitment.

For 15 years Daeng Xayaseng has been travelling through rugged, undulating countryside by motorbike and by foot to deliver vaccines to children in some of the most remote villages in Laos.
It’s hard work but she is determined: “We have a target of children to reach and we’ll achieve that no matter how long it takes,” she says. “We’ll keep working until we reach every child.”
Today her team visits Nampoung village, 4 hours north of the capital of Laos, to deliver polio vaccines.
“For 15 years I’ve been working on campaigns like this,” she says. “Today we’re here with our outreach team to vaccinate children against polio. We’ll also go house to house to make sure no child misses out on being vaccinated.”
“We don’t want there to be another outbreak of polio so we have to reach everyone,” says Daeng. “In order to do that, immunizing every child in remote communities like this is a priority to ensure everyone is protected.”
UNICEF and other partners of the Global Polio Eradication Initiative are supporting the Lao Government to reach nearly half a million children under five with potentially life-saving vaccines. More than 7,200 volunteers and 1,400 health workers like Daeng and her team have been mobilized to deliver the oral polio vaccine as well as other vaccinations such as measles-rubella.
“I’m very happy and proud to do this job,” says Daeng once the team has packed up. “I’m proud to do this job to serve the community and help in any way I can.”

Read more:
A vaccine manufacturer in Stockholm has taken the first step towards becoming a certified Poliovirus Essential Facility (PEF), leading the charge in global efforts to safely and securely contain type-2 poliovirus. This facility has been awarded a Certificate of Participation co-signed by the National Authority for Containment (NAC) in Sweden and the Global Commission for the Certification of Poliomyelitis Eradication (GCC). The Certificate is the first of its kind to be issued, indicating formal engagement in the global containment certification process.
Wild poliovirus type-2 was declared eradicated by the GCC in September 2015, however, there is risk of the virus resurging. Following the removal of the type-2 component from oral polio vaccine (OPV) and the discontinuation of type-2 containing OPV from routine use in April 2016, countries around the world have been asked to safely and securely destroy their type-2 polio samples. As a further precaution, countries continue to immunize against type 2 polioviruses with inactivated polio vaccine. For facilities needing to retain the virus for vaccine production or for critical research, stringent containment measures need to be followed. The first step is getting a Certificate of Participation.
“We are pleased to see Sweden leading the way in demonstrating conforming with the processes to minimize the risk of releasing type-2 poliovirus into the environment. Participation in the Containment Certification Scheme shows that both the facility and the host country are serious about taking on and implementing the safeguard measures necessary to become a PEF,” said Prof. David Salisbury, Chair of the GCC and of the Commission’s European regional body.
“Handling and storing an eradicated pathogen is a risk and responsibility – a leak or breach could have devastating consequences,” said Michel Zaffran, Director of Polio Eradication at the World Health Organization. “We commend Sweden for its commitment towards ensuring safety standards are met and protocols are in place to help minimize risk, and for paving the road for the containment certification process,” he said.
“The issuance of a Certification of Participation formally engages a designated PEF in the containment process. Provided that the facility meets the requirements outlined in Global Action Plan III for the containment of polioviruses (GAPIII) within given time frames, it can then progress to achieving an Interim Certificate of Containment and finally, a full Certificate of Containment to become an accredited PEF,” said Prof. Salisbury. “Countries planning to retain type-2 poliovirus will need to establish their NACs as soon as possible, and by no later than the end of 2018. The GCC urges all countries that plan to have PEFs to get the ball rolling in this process,” he said.
Since April 2016, most facilities around the world have opted to destroy their type-2 poliovirus materials rather than contain them. Twenty-nine countries, however, plan to continue to handle and store their materials in 92 designated PEFs.
WHO will propose a resolution for consideration by the World Health Assembly in May to seek international consensus on accelerating containment efforts globally.

From the front passenger seat of a small utility truck, Mahmoud Al-Sabr hangs out the window, looking for families and any child under five years old to be vaccinated against polio. As the car he travels in dodges rubble and remnants of buildings that once stood tall in Raqqa city, he flicks the ‘on’ switch for his megaphone.
“From today up to January 20, free and safe vaccine, all children must be vaccinated to be protected from the poliovirus that hit Syria for the second time,” he calls, beckoning families with young children who have recently returned to Raqqa city to come outside of their makeshift homes amongst destroyed buildings, to have their children vaccinated.
In 2017, amidst the protracted conflict and humanitarian crisis in Syria, an outbreak of circulating vaccine-derived poliovirus type 2 (cVDPV2) was detected, threatening an already vulnerable population.
Due to ongoing conflict, Raqqa city, which was once host to half of the governorates population, had been unreached by any vaccination activity or health service since April 2016. During the first phase of the outbreak response, more than 350,000 resident, refugee and displaced children were vaccinated against polio in Syria, but “Raqqa city remained inaccessible,” says Mahmoud.
In January 2018, polio vaccinators conducted the first vaccination activity in the city since it became accessible again, following the end of armed opposition group control.
There were no longer accurate maps or microplans that vaccinators could use to guide them in their work. Unrecognizable, the city was a picture of devastation with few dwellings untouched by the violence that once caused families to flee. The house-to-house vaccination campaign that usually helps the programme to reach every child under five wouldn’t work here. Teams knew they would have to innovate to seek out families wherever they were residing to vaccinate their children.
“All children must be vaccinated to protect against poliovirus,” Mahmoud echoes around shelled out buildings, and slowly mothers and fathers carrying their children start to appear in the street.
Mahmoud and Ahmed Al-Ibraim are one of 12 mobile teams that are going street by street, building by building, by car in search of children to vaccinate. Carrying megaphones to alert families of their presence and to tell them of the precious vaccines they carry that will protect their children from the paralysing but preventable poliovirus, they slowly cover areas of the city now unrecognizable.
“No one could enter Raqqa City now for two years,” says Abdul-Latif Al-Mousa, a lawyer from the city who joined the outbreak response as a Raqqa City supervisor for polio campaigns. “So children have not been vaccinated here since that time. Now that people have returned, we are learning where they have returned from and we vaccinate them regardless.”
“We must reach each child with the vaccine to protect them – polio is preventable, why should they suffer more?” Ahmed appeals.
Campaign brings vaccines and familiar faces
Vaccines were not the only thing to return to Raqqa City in January. It was the first time that WHO polio focal point Dr Almothanna could return to Raqqa City after being force to flee under the rule of the armed opposition group. Imprisoned for refusing the demands of the group, friends and neighbours of Dr Almothanna facilitated his escape from the city in 2016.
Dissatisfied but not deterred, Dr Almothanna continued to work with the polio programme, serving the whole governorate except his own city. Over the course of the January 2018 campaign, he worked tirelessly with vaccination teams to ensure more than 20 000 children under the age of five in Raqqa City received a dose of mOPV2 to protect them against polio. For many, it was the first vaccination they had received. In the additional campaigns that followed in March 2018, even more children were reached.
The microplans developed by vaccinator teams in the first vaccination round have become a critical road map for reaching children and families with health services, accounting for the locations of returned families and information about neighbouring families that teams had not yet located. In the second round, the microplans were updated to include new families who had returned.
Syria reported 74 circulating vaccine-derived poliovirus cases between March and September 2017. It has been more than six months since the last case was reported (21 September 2017). Efforts are continuing to boost immunity in vulnerable populations, maintain sensitive surveillance for polioviruses and strengthen routine immunization to enhance the population immunity.

Forty-year-old Auta A. Kawu says the only thing predictable about working in the conflict-affected northeastern Nigerian State of Borno is its unpredictability.
“No two days in my week are alike,” he says.
As a Vaccine Security and Logistics facilitator, Auta is one of 44 specialists working with the Government, UNICEF and partners in Nigeria, who strive to ensure sufficient vaccine stock, appropriate distribution and overall accountability for vaccines in the country. Through careful management, Auta works to give every accessible child in Borno protection from vaccine-preventable diseases, including polio.
Describing a typical week in his life, he explains that if on Monday he is arranging for the vaccination of eligible children among a group of Nigerians returning back from neighbouring countries where they had fled due to fear of violence, by Tuesday he could be speaking with government personnel to find a way to safely send vaccines to security compromised areas. On Wednesday, he may find himself rushing extra vaccines to an internally displaced persons (IDP) camp, where more people have arrived than initially expected, whilst on Thursday you may find him trying to locate a cold chain technician to fix a fridge where the heat-sensitive polio vaccine must be stored.
Evidencing the energy and commitment required to work on the frontline of vaccination, Auta notes that the work never lets up. Despite an exhausting week, on a typical Friday, you might find him on the road again, travelling to a remote location where health workers have just been given access. When he gets there, he will help out once more – trying to ensure that vaccines are distributed as effectively as possible to maximize the number of children reached.
He recounts a recent story of reaching the reception area of an IDP camp in Dalori, which is located in a highly volatile area of the state. Arriving with 300 doses of oral polio vaccine, and 200 doses of measles vaccine, he was told that new arrivals were expected later that day. Many of the people coming had been under siege by non-state armed groups since 2016, and had taken the opportunity of improved security and mobility to flee to the nearest town. Very few of the young children arriving had ever been reached with vaccines.
With the screening of children eligible for measles and polio vaccines starting around 9 am, and plenty more children yet to arrive, it was quickly clear that the available doses would not be enough.
Springing into action, Auta notified the head of the security team accompanying him of the need to go to nearest health facility to bring additional doses. Once clearance was given, he rushed to Jere Local Government, a district nearby, to collect more vaccines.
In the meantime, however, there were sudden changes in the security environment. The return journey to Dalori was not cleared until late noon.
Luckily, giving up isn’t in Auta’s nature.
By the end of the day, he had successfully delivered 580 doses of oral polio vaccine and 460 doses of measles vaccines for the children in the camp, providing some of them with their first ever interaction with a health system.
The crucial role of Vaccine Security and Logistics facilitators like Auta cannot be over-emphasized. In addition to his central work, Auta also conducts advocacy visits to traditional and religious leaders and supports the planning and implementation of vaccination campaigns in inaccessible areas.
Vaccine facilitation may be unpredictable work, but Auta is secure on one thing. Thanks to the work of him, and thousands of other determined health workers, community mobilizers and with support from donors and partners including the Bill & Melinda Gates Foundation, the Government of Canada, the Dangote Foundation, the European Union, Gavi – The Vaccine Alliance, the Government of Germany, the Government of Japan, the Japan International Cooperation Agency (JICA), Rotary International, the US Centers for Disease Control and Prevention, the World Bank and others, Nigeria is steadily on its way to being declared polio-free.


Welcome to Poliopolis! You’ll spend the next 28 days in a container village to help us test a new polio vaccine. Poliopolis is equipped with all the amenities to make your stay comfortable: air-conditioned private rooms with workstations and sinks, a lounge area with a flat screen TV and foosball table, a fitness room with a variety of exercise equipment, and a bright, sunny dining area. Enjoy your stay!
Sounds like a scene from a science fiction story, right? But this is a real polio vaccine trial that took place in a parking lot at the University of Antwerp, Belgium in mid-2017. The study, funded by the Bill and Melinda Gates Foundation, evaluated two novel oral polio vaccine candidates. These vaccine candidates were developed by scientists from the US Centers for Disease Control and Prevention’s polio laboratory, the National Institute for Biological Standards and Control in the United Kingdom, and the University of California, in San Francisco, with support from the US Food and Drug Administration.
Once fully developed and tested, these new, more genetically-stable, live, attenuated vaccines will prove a critical resource to ensure global polio eradication.
Read more:
US Centers for Disease Control and Prevention – Welcome to Poliopolis
Ondrej Mach of the WHO polio research team discusses why new inactivated polio vaccine solutions are needed for the post-eradication era. Why are we developing entirely new vaccines for a disease which will no longer exist?
In March, the Afghanistan polio eradication initiative conducted its first nation-wide immunization campaign for polio eradication in 2018. In just under a week, around 70 000 workers knocked on doors and stopped families in health centres, city streets and at border crossings to vaccinate almost ten million children. What an incredible achievement.
But what does a huge campaign like this take?
We had a look behind the scenes and followed the week in Herat, western Afghanistan. See what the campaign looked like from beginning to end through this photo essay.

In Afghanistan, frontline health workers explain to parents why the polio vaccine must be delivered multiple times
“It’s easy for the others, they are young and strong!” laughs Hamida. She has just climbed hundreds of steps to the top of a long and steep staircase on the side of one of Kabul’s many hills. Together with her colleagues Mohib and Khalid she works as a part of a polio team vaccinating children in their community. Today, the team started at 8 am, and they have now been walking up and down the hill for three hours. No wonder she is tired.
So far, the group has visited 50 families and vaccinated 110 children. They have 30 more to go today, and, in the next three days, they will visit a total of 233.
The team’s role is not only to vaccinate the children but to also to educate people about the life-saving polio vaccine and its importance. It is not always an easy job.
“Last time we visited was only two weeks ago, so some parents have been asking why we are visiting again. I have explained to everyone that the vaccine is beneficial for the children and that children need to be vaccinated every time we visit to be protected.”
It is the first day of a vaccination campaign, which aims to immunize over 6 million children against polio in Afghanistan.
Today, thankfully, all families have accepted the vaccine from this team.
Last push to eradicate polio in Afghanistan
Afghanistan is one of the last countries in the world where wild poliovirus still circulates, and has the highest number of children paralyzed by the virus.
In 2017, there were a total of 14 cases and, so far in 2018, there have been three confirmed cases. In recent months, the virus has been found circulating in southern and eastern regions.
WHO Afghanistan polio programme manager Dr Hemant Shukla is confident that with stepped-up efforts, the circulation can be stopped. “Afghanistan has stopped transmission in the past in all areas, but not at the same time. We are confident that by following correct strategies, focusing in the right areas and by coordinating our efforts with neighbouring Pakistan, we can stop the transmission”.
To answer to the challenge, the Polio Eradication Initiative has stepped up efforts to detect any viruses in the environment. The programme is taking special steps in the eastern and southern regions to reach all children with the vaccine every time the vaccinators pass by, as these are very high risk areas for polio transmission, with people moving in and out of neighbouring Pakistan. Special outreach tactics are concurrently aiming to reach and immunize ‘mobile populations’, such as nomadic people, who are at high risk of contracting polio.
The oral polio vaccine is effective as it not only protects children from contracting the virus, it also prevents them from carrying it in their intestines. Several doses – spaced apart – need to be given to build sufficient immunity, especially in areas where poor nutrition can weaken immune systems.
During the low transmission season, the Polio Eradication Initiative conducted two campaigns – in January and February – in order to vaccinate children in high risk and very high risk districts in quick succession so that the vaccine would have a maximum effect.
In March, 10 million children across the whole country will be vaccinated – that’s every single child under the age of five years.
In Kabul, one by one the team marks their tally sheet with numbers and ages of the children and takes note whether all the children of the household were present.
One of the children vaccinated today is three-year-old Haroon, who stands outside his family’s home. His mother Nadia peeks through the gate. She has six children, and Haroon is her youngest.
“Haroon was just vaccinated two weeks ago, but I know it is important to vaccinate children every time”.
The team marks this household vaccinated for today.
In four weeks, Nadia will open up her door when the vaccinators knock again.

Reducing polio cases by 99.9% globally is an incredible feat, achieved through innovative strategies and years of trial and error.
While the polio eradication programme is focused on getting to zero, now is the time to make sure everything we’ve learned isn’t lost and can be used to inform future global health programmes. Just as the polio eradication effort applied lessons learned from the successful smallpox campaign to its own work, the goal is for future health programmes to understand and build on the knowledge of the polio effort.
Under a new grant from the Bill & Melinda Gates Foundation, the Johns Hopkins Bloomberg School of Public Health (JHSPH) will be working to do exactly this.
JHSPH will partner with academic institutions from around the world to document lessons and develop graduate-level courses and hands-on training clinics for public health students and professionals, including an online open course available to the public and implementation courses for managers from other health programmes.
Under the leadership of Dr Olakunle Alonge, the team at JHSPH will collaborate with a global team from public health institutions in seven countries: Nigeria, India, Afghanistan, Ethiopia, the Democratic Republic of the Congo, Bangladesh and Indonesia. This will not only ensure a balanced and diverse perspective, but also enable the exchange of public health training strategies between the institutions.
To develop the content of each course, JHSPH will be identifying “change agents” at the local, national and global levels who have expertise in polio eradication that may not otherwise be captured. This unique global strategy promises to yield coursework that speaks to the issues faced by a broad range of global health programmes and actors.
“Without an active strategy to map, package and deliver the knowledge from the global polio eradication efforts to other programs and global health actors, I’m afraid that these knowledge assets may not find any useful purpose beyond the end of the polio campaign, which could come to an end within a few years,” said Alonge.
Alonge expects to glean lessons that will apply to immunization systems, public health emergency response, primary health care, disease eradication and infectious diseases—ensuring that the polio programme continues to positively impact global health for years to come.
Read more